About Glaucoma


Most common form of glaucoma in the US (angle-closure much more common in Asia)
Can be associated with high or low intraocular pressure ("low-tension glaucoma"). There is no "normal" range for intraocular pressure. The concept of "normal pressure" being between 10 and 21 mm Hg is out of date.
Patients can have glaucoma at low pressure or no damage at all with high pressure (ocular hypertension)
The internal drainage system of the eye, the trabecular meshwork, becomes clogged and can lead to optic nerve damage
Having a higher eye pressure tends to be a risk factor to develop glaucoma
Central corneal thickness (CCT) measurement can affect the accuracy of the pressure measurement and risk of damage
Diagnosed by a pattern of damage to the optic nerve
Side or peripheral vision is typically lost first, then central vision if not adequately treated
Glaucoma does not usually have symptoms and can progress even to advanced stages without the patient becoming aware. Regular complete eye exams are the best way to diagnose glaucoma. At the point that a patient can notice a blind spot ("scotoma") or loss of vision, the damage is very advanced
Patients can have glaucoma and still have a normal visual field; this is early glaucoma
Treatment can be eye drops, laser trabeculoplasty or surgery, or a combination and is decided with the patient on an individualized basis
A treatment goal "target pressure" or range is given based on the patient's individualized risk factors, such as degree of damage, CCT and age, and can be adjusted along the course of treatment
Treatment is usually lifelong
Surgery (trabeculectomy is the most common) may control but not eliminate the glaucoma, may not last the patient's lifetime or drops may be needed in conjunction, but is often the most definitive way to lower the eye pressure
Glaucoma status is monitored by eye pressure checks, visual field testing, optic nerve exam, and optic nerve imaging on a long-term basis

Commonly associated with being farsighted ("hyperopia")/having a shorter eye and/or cataract development
Diagnosed by gonioscopy as part of the eye exam
Commonly runs in families; family members who are adult and have not had cataract surgery should inform their eye care provider of this part of the family history
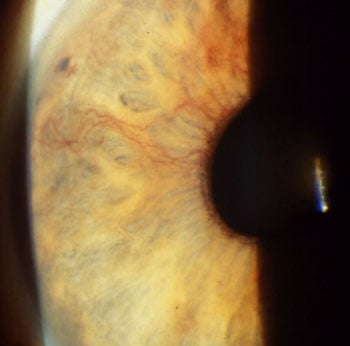
The width of the angle leading to the trabecular meshwork (internal drainage system) becomes narrower with age
If the drainage system becomes narrow enough to close off, acute angle-closure may develop; this is usually preventable with laser iridotomy (see bottom photo)
Once laser iridotomy is performed and confirmed open, medications with the glaucoma warning can be used (rare exception - plateau iris syndrome)
Angle-closure glaucoma can be slow/chronically progressive, not just appear as acute angle-closure
Angles can also close slowly and silently by development of adhesions and can cause chronic angle-closure glaucoma.
Overproduction of elastic tissue inside the eye, can be isolated finding as a risk factor for glaucoma, or lead directly to glaucoma
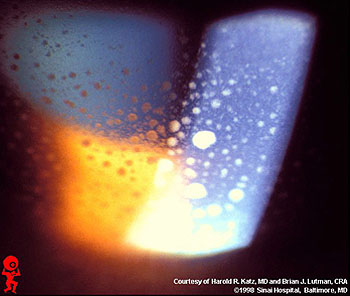
Dandruff-like particles on the margin of the pupil and the front surface of the lens
50% of patients have or develop pseudoexfoliation in both eyes, although one eye may be several years ahead of the other eye
Of those with pseudoexfoliation, 50% will develop glaucoma
Commonly associated with a family history of glaucoma or ocular hypertension, but necessarily specifically pseudoexfoliation
Can make cataract surgery more difficult - the pseudoexfoliation material deposits on the zonules of the lens (which function like ligaments) and can weaken them, increasing the chance of the lens dropping to the back of the eye or vitreous jelly coming forward within the eye
May be associated with poor pupil dilation as the pseudoexfoliation material deposits within the iris, further increasing difficulty with cataract surgery
Tends to be a more volatile type of glaucoma, initially responding to treatment but then escaping control
May be associated with very high intraocular pressures, either chronic or spiking
Tends to respond well to laser trabeculoplasty
Commonly associated with narrow angles and angle-closure

Most common in younger, nearsighted patients
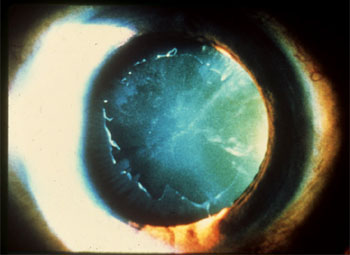
Characterized by the iris bowing backward, causing pigment from the back of the iris to rub off and clog up the trabecular meshwork (internal drainage system of the eye)
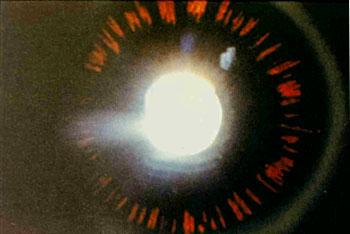
Typical findings are a Krukenberg spindle (the pattern that pigment deposits on the back of the cornea), iris transillumination defects and very heavily pigmented trabecular meshwork
May cause blurred vision with exercise
Responds very well to laser trabeculoplasty
Some patients who have "reverse pupillary block" may respond to laser iridotomy
Some patients will actually outgrow this type of glaucoma
Commonly associated with a family history of glaucoma or ocular hypertension, as well as pigmentary glaucoma
Many patients will have pigment dispersion syndrome, with the findings of the iris transillumination and Krukenberg spindle, but no glaucoma. These patients should have more frequent eye pressure checks to watch for the development of elevated intraocular pressure
Patients may be on a spectrum, having the above findings, with ocular hypertension but no glaucoma damage
Inflammatory glaucoma; a very wide spectrum
The eye pressure can become very high from inflammatory cells blocking the trabecular meshwork (internal drainage system)
Uveitis can involve only the front of the eye (iritis), the back of the eye, or the entire eye
Can be only one eye or both eyes
If both eyes, can be the same or different times for involvement
Can be a single episode, recurring episodes or chronic
50% of iritis never has an underlying cause found
Can be caused by an inflammation inside the eye alone, or associated with an autoimmune or infectious disease
May require blood tests, chest xray and/or skin testing for TB to look for an underlying cause
Treatment of the inflammation is the first priority, as that alone may reduce the eye pressure. If the eye pressure is still high after or while managing the inflammation, eye drops or surgery could be required
Can be sudden or slow onset
Not usually an inherited type

"Neo" = new, "Vascular" = vessel; glaucoma caused by new blood vessels
Typically managed in conjunction with a retina specialist and medical doctor
Caused by lack of oxygen to the retina
Most common causes are diabetes, central retinal vein or artery occlusion (stroke to the eye) or carotid artery disease
When the retina does not get enough oxygen, it produces a chemical called VEGF, which builds new blood vessels. The system is faulty and the new blood vessels break, pull and bleed. When the VEGF chemical signal is strong, new blood vessels grow in the iris and create a membrane that seals over the trabecular meshwork (internal drainage system)
The glaucoma can come on very suddenly, unlike open-angle glaucoma, and cause severe pain and nausea from very high eye pressure
Not an inherited type
Treament is a combination of retinal laser and possibly injections of anti-VEGF medication along with glaucoma treatment. Eye drops for glaucoma do not usually work well in this setting and a procedure is commonly needed to control the eye pressure. Laser trabeculoplasty is not an option. Trabeculectomy has a higher rate of failure and eyes with decent vision or potential vision are most likely to need a tube shunt (
 Baerveldt or
Baerveldt or  Ahmed Valve). Eyes which have permanently lost vision and need lower pressure for pain control may get a diode laser transcleral cyclophotocoagulation. The diode laser may be done in the office or in the operating room under sedation per patient preference.
Ahmed Valve). Eyes which have permanently lost vision and need lower pressure for pain control may get a diode laser transcleral cyclophotocoagulation. The diode laser may be done in the office or in the operating room under sedation per patient preference.Even if the intraocular pressure becomes controlled, the patient's vision depends on the status of the retina
 Ocular Hypertension
Ocular Hypertension
Statistical elevation of intraocular pressure, though confusing as there is no "normal" range for intraocular pressure
Higher pressure has been shown to be a risk factor for the development of glaucoma in many studies, the most recent of which is the Ocular Hypertension Treatment Study (OHTS)
Central corneal thickness (CCT or pachymetry), measured as part of the exam (usually a single-time measurement), can affect the accuracy of the intraocular pressure reading. The cornea is the clear front portion of the eye.
The eye pressure is measured with a "tonometer" which is calibrated to an average corneal thickness of 545 microns (one one-thousandth of a mm). The pressure is the force neccesary for the tonometer to indent the central 3.06 mm of the cornea to a specific position. A thin cornea will take less force to indent the cornea and the eye pressure will be read lower than it truly is; a thick cornea will take more force to indent and overread the true pressure. The true pressure does not have an exact "correction factor" but is more of a "thin, thick or average" to consider along with the actual pressure reading
Risk calculation" has been created, using specific patient and exam components to help determine who should start pressure-lowering treatment and is adjusted according to an individualized plan
 Glaucoma Suspect
Glaucoma Suspect
Usually used to describe a patient with a "suspicious" appearing optic nerve, normal visual field and absence of specific changes to the optic nerve such a localized tissue loss
The optic nerve is graded by the "cup-to-disc ratio" (C/D), meaning what proportion the central space or cup takes up of the entire optic nerve head "disc" space
There is no cutoff for normal which is why many patients fall into the "suspicious" category
The size of the optic nerve itself is an important component. A larger C/D has been shown to be a risk factor for glaucoma. However, a larger optic nerve itself is actually born with more nerve fibers as well as a larger cup, so it can be difficult to determine who is normal vs. having glaucoma as there can be considerable overlap. Patients may be born with naturally large cups and not have glaucoma or could be born with a small cup which enlarges and is true glaucoma; a change in the optic nerve is more significant than actual C/D
Patients are typically monitored by visual field testing, complete eye/optic nerve exam and optic nerve imaging
Treatment vs. monitoring without treatment is determined on an individual basis
A patient with a severe family history of glaucoma should be followed as a glaucoma suspect
Glaucoma Consultants
6565 N. Charles St, Suite 302, Baltimore, MD 21204

Phone:  410-825-9225
410-825-9225
Fax: 410-825-9229
Monday to Friday: 8:00 AM – 5:00 PM
Saturday to Sunday: Closed